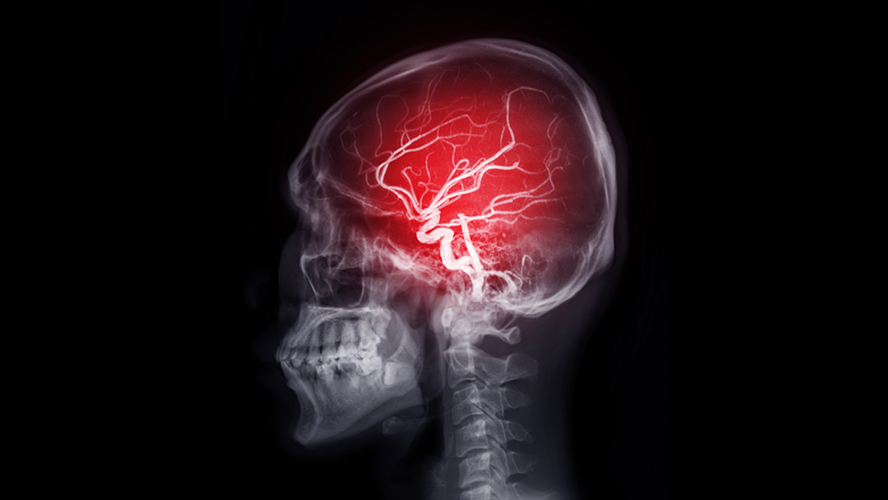
A team led by Dr. Philippe Monnier at UHN’s Krembil Brain Institute (KBI) has uncovered a promising new target that could help limit brain injury following an ischemic stroke—a type of stroke caused by a blood clot.
In a healthy brain, the blood-brain barrier acts like a filter, controlling which substances can enter or leave the brain, thereby protecting the brain from harmful substances. After a stroke, some proteins—like one called RGMa—can change the structure of blood vessel walls in the brain. These changes compromise the vessels’ integrity and make them more permeable, or “leaky”, allowing harmful substances in the blood to enter the brain where they cause damage.
The proteins responsible for these changes must first be activated by enzymes such as pro-protein convertases (PPCs). These enzymes act like a switch to turn on other proteins. While PPC inhibitors have been used in other diseases, and blocking RGMa has shown benefits in stroke models, scientists still don’t fully understand how PPCs affect stroke. Among PPCs, subtilisin kexin isozyme-1 (SKI-1) is one of the least understood, but it may play a key role in how blood vessels respond after stroke.
To study SKI-1’s role, the team used preclinical stroke models and blocked the enzyme with a drug called PF-429242. The results were promising: genes that help keep blood vessels strong became more active, while those linked to damage were turned off. Inhibition of SKI-1 also resulted in reduced cell death and smaller areas of brain tissue damage. Importantly, these changes led to better brain function in models.
Building on these findings, the team also discovered that removing a protein called Neogenin had similar protective effects as blocking SKI-1. Without Neogenin, RGMa couldn’t make the blood vessels leaky.
These findings shed light on the molecular mechanisms that contribute to brain damage after ischemic stroke, specifically the role of RGMa, Neogenin, and SKI-1 in compromising blood-brain barrier integrity. By identifying SKI-1 and Neogenin as potential therapeutic targets, this research opens the door to new treatment strategies aimed at protecting brain tissue and improving cognitive outcomes. With further validation in human studies, these discoveries could pave the way for more effective, targeted therapies that transform stroke recovery and reduce long-term disability.
Dr. Alireza Shabanzadeh is the first author of this study. He is a scientific associate in the Monnier Lab at UHN’s Krembil Brain Institute.
The senior author of this study is Dr. Philippe Monnier, a Senior Scientist at UHN’s Krembil Brain Institute and a Professor in the Department of Physiology in the Temerty Faculty of Medicine at the University of Toronto.
This work was supported by the Canadian Institutes of Health Research, the Heart and Stroke Foundation, and UHN Foundation.
The authors declare no competing interests.
Shabanzadeh AP, Ringuette D, Syonov M, Wu Q, Tassew NG, Mun EK, Meek A, Lively S, Suntharalingham SE, Mojica M, Olijnyk L, Qiang B, Foltz WD, Reed M, Moya I, Brown C, Feng J, Qin X, Akula PS, Wälchli T, Carlen PL, Alcaide-Leon P, Monnier PP. Inhibition of proprotein convertase SKI-1 prevents blood vessel alteration after stroke. Nat Cardiovasc Res. 2025 Sep;4(9):1094-1113. Epub 2025 Aug 26.




