A new study from UHN's Toronto General Hospital Research Institute (TGHRI) and Princess Margaret Cancer Centre (PM) has found that a mix of gut bacteria, called MET4, can trigger an immune response in patients with cancer receiving immunotherapy. This finding deepens our understanding of how gut microbes may affect the immune system as it fights cancer.
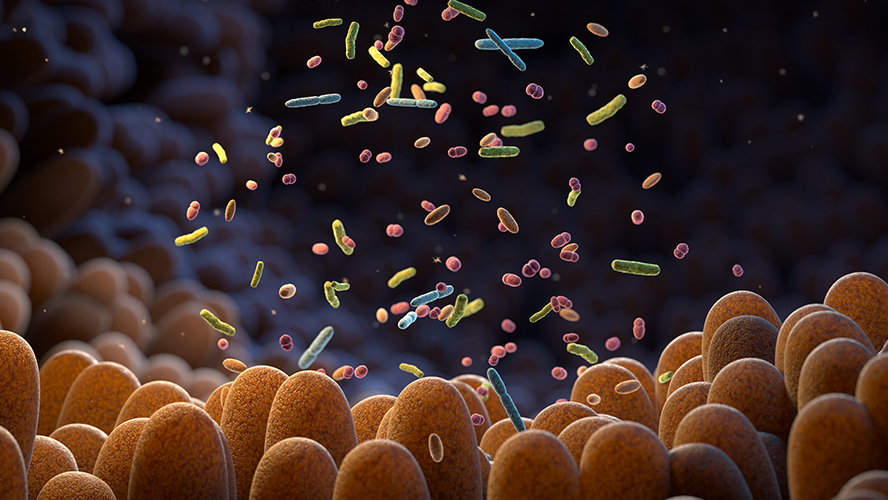
The gut microbiome—a complex community of bacteria, viruses, fungi, and other microbes—has been shown to influence how well cancer treatments work. However, scientists still do not fully understand how this happens. Recent studies combining microbial treatments like fecal microbiota transplants (FMT) with cancer immunotherapy have shown promising results and are areas of active investigation and clinical trials.
Compared with FMT, treatments made from specific groups of bacteria—called bacterial consortia—are considered safer, more consistent, and easier to scale up for clinical use. One such treatment, MET4 (Microbial Ecosystem Therapeutic 4), is a novel microbial mixture of 30 gut bacterial species. Early trials showed that it is safe and well-tolerated when given with immunotherapy.
In a previous study, patients who received both FMT and immunotherapy developed specific antibodies against the added bacteria. These antibodies were linked to better responses to immunotherapy. This suggests that the presence of these antibodies could be an indicator that the immune system is fighting cancer and that the treatment is working.
To test if MET4 would create a similar immune response, Drs. Bryan Coburn, Senior Scientist at TGHRI and Anna Spreafico, Clinician Investigator at PM, and their teams analyzed patient blood and fecal samples before and after treatment. They found that MET4 triggered antibody production against the bacteria in the mixture, and that these changes only occurred in people who received MET4.
In patients who responded well to the treatment, the team also saw more beneficial gut bacteria, changes in immune cells like B and T cells, and a decrease in inflammatory monocytes, suggesting that the immune system behaved differently.
These findings suggest that microbial therapies like MET4 might boost the immune system during immune-targeting cancer treatments. Further investigation on how different mixes of bacteria affect the immune system using similar assessments will aid in designing optimal microbial treatments to help boost cancer therapies.
Dr. Matthiew K. Wong, Postdoctoral Researcher at UHN, is the first author of the study.
Dr. Bryan Coburn, Senior Scientist at Toronto General Hospital Research Institute and Associate Professor in the Departments of Medicine and Laboratory Medicine & Pathobiology at the University of Toronto, is co-senior author of the study.
Dr. Anna Spreafico, Clinician Investigator and Medical Oncologist at Princess Margaret Cancer Center and Associate Professor in the Department of Medicine, is the co-senior author of this study.
This work was supported by the Conquer Cancer-the ASCO Foundation, the American Society of Clinical Oncology (ASCO), NuByiota, Tomczyk Microbiome Initiative Fund, The Princess Margaret Cancer Foundation, and UHN Foundation.
For a list of competing interests, please see the manuscript.
Wong MK, Boukhaled GM, Armstrong E, Liu R, Heirali AA, Yee NR, Tsang J, Spiliopoulou P, Schneeberger PHH, Wang BX, Cochrane K, Sherriff K, Allen-Vercoe E, Siu LL, Spreafico A, Coburn B. Microbial Ecosystem Therapeutics 4 (MET4) elicits treatment-specific IgG responses associated with changes in gut microbiota in immune checkpoint inhibitor recipients with advanced solid tumors. J Immunother Cancer. 2025 Mar 22;13(3):e010681. doi: 10.1136/jitc-2024-010681.




