Researchers at the University Health Network have identified a new target that may increase the effectiveness of cancer immunotherapy by focusing on the metabolism of T cells.
Immunotherapy has been a major game changer in the treatment of cancer. Nonetheless, some tumors fail to respond to the treatment, which has prompted researchers to search for new ways to improve its effectiveness.
Studies have shown that metabolic and energetic processes within T cells are linked to their ability to kill cancer and inhibit tumor growth. Therefore, leveraging these processes may be a promising approach to enhance the efficacy of immunotherapy.
To understand this further, a team led by Dr. Pamela Ohashi, Senior Scientist and Director of the Tumor Immunotherapy Program at the Princess Margaret Cancer Centre, performed an in depth analysis of the metabolic pathways in three different subsets of T cells with varying anti-tumor properties.
They discovered that T cells with the strongest anti-tumor activity had an increased expression of a metabolic pathway known as the pantothenate/coenzyme A (CoA) pathway.
Treating T cells with CoA led to an increase in their energy-production and enhanced their anti-tumor function.
“The discovery that a single molecule involved in metabolism can have a profound impact on the function and anti-tumor activity of a T cell was an exciting finding,” explains Dr. Michael St Paul, postdoctoral fellow and co-first author of the study.
Further, in preclinical experimental models, treatment with the pantothenate, a precursor to CoA, was able to improve the effectiveness of immunotherapy and increase overall survival.
“To determine if these findings were applicable in the clinical setting, we looked at these pathways in advanced melanoma patients,” says Dr. Sam Saibil, Medical Oncologist and co-first author of the study. “What we found was that those patients with higher blood levels of pantothenate prior to undergoing treatment, had a better response to immunotherapy.”
“This work revealed a new role for the pantothenate/coenzyme A (CoA) pathway in promoting anti-tumor immunity and lays the foundation for future studies that explores whether manipulating this metabolic pathway in T cells can improve the efficacy of immunotherapies,” says Dr. Ohashi.
This work was supported by the Canadian Institutes of Health Research, the Natural Sciences and Engineering Research Council of Canada and The Princess Margaret Cancer Foundation. Dr. Trevor Pugh holds a Tier 2 Canada Research Chair in Translational Genomics. Dr. Pamela Ohashi is a Professor of Immunology at the University of Toronto and holds a Tier 1 Canada Research Chair in Autoimmunity and Tumour Immunity.
St. Paul M, Saibil SD, Han SJ, Israni-Winger K, Lien SC, Laister RC, Sayad A, Penny S, Amaria RN, Haydu LE, Garcia-Batres C, Kates M, Mulder DT, Robert-Tissot C, Gold MJ, Tran CW, Elford AR, Nguyen L, Pugh TJ, Pinto DM, Wargo J, Ohashi P. Coenzyme A fuels T cell antitumor immunity. Cell Metab. 2021 Dec 7. DOI: 10.1016/j.cmet.2021.11.010.
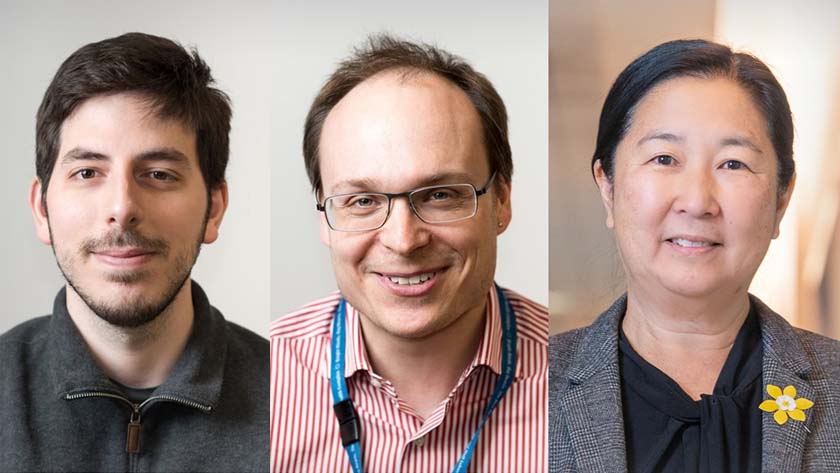
(Left to right) Dr. Michael St Paul, Postdoctoral Fellow; Dr. Sam Saibil, Staff Oncologist at the Princess Margaret Cancer Centre; and Dr. Pamela Ohashi, Senior Scientist and Director of the Tumor Immunotherapy Program at the Princess Margaret Cancer Centre. Drs. St Paul and Saibil are co-first authors of the study.




