Some bacteria, viruses and fungi are like unwelcomed guests who crash a party and cause trouble. Without an invitation, they discreetly slip into the body where they cause an infection that damages tissues and threatens a person’s health.
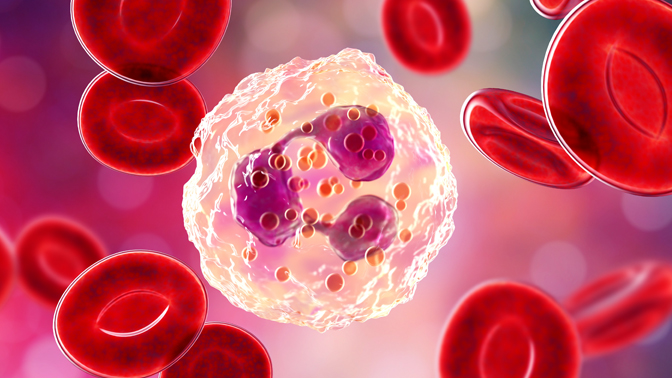
Luckily, the body is staffed with immune cells—known as neutrophils—responsible for removing these party crashers. Neutrophils have several tactics at their disposal to eliminate microscopic invaders, including the release of neutrophil extracellular traps (NETs). NETs are web-like structures of DNA and proteins that bind, disarm and kill invaders.
“Although NETs are a powerful weapon in the fight against infections, accumulating evidence suggests that NETs might also contribute to the spread of a cancer to other sites in the body,” says Dr. Scott Bratman, a Scientist at the Princess Margaret Cancer Centre.
Recently, Dr. Bratman and his colleagues published a report describing a series of experiments that helped clarify the importance of NETs in this process.
They discovered that high blood levels of toxic molecules known as reactive oxygen species (ROS) triggered the release of NETs from neutrophils in the absence of microscopic invaders. They also found that NETs accumulated in the lungs more than in any other organ.
Next, the researchers examined how high ROS levels and NETs affected experimental models of breast cancer, and head and neck cancer. They found that when ROS levels were high, both cancers were more likely to spread to the lungs.
The researchers also obtained evidence suggesting that this phenomenon occurs not only in experimental models of cancer, but also in cancer patients. ROS levels were found to be much higher in head and neck cancer patients whose cancer eventually spread to their lungs.
Commenting on his findings, Dr. Bratman says, “We found that cancer can spread to the lungs by using NETs released in response to high ROS levels. Because of this, we believe that ROS could represent a new and promising anticancer target that could help stop the spread of cancer.”
This work was supported by The Terry Fox Foundation and The Princess Margaret Cancer Foundation. M. Ikura holds a Tier 1 Canada Research Chair in Cancer Structural Biology.
Inoue M, Nakashima R, Enomoto M, Koike Y, Zhao X, Yip K, Huang SH, Waldron JN, Ikura M, Liu FF, Bratman SV. Plasma redox imbalance caused by albumin oxidation promotes lung-predominant NETosis and pulmonary cancer metastasis. Nat Commun. 2018 Nov 30. doi: 10.1038/s41467-018-07550-x.

Dr. Scott Bratman, Scientist, Princess Margaret Cancer Centre.




