Findings from the Princess Margaret Cancer Centre showcase a new approach for treating acute myeloid leukemia—an aggressive cancer of the blood that is known to return following standard treatments.
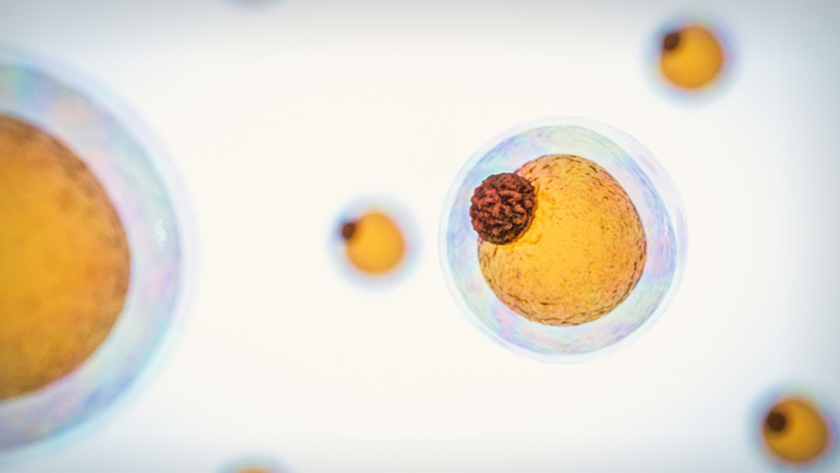
Recurrence of this cancer is driven by leukemic stem cells. These cells are often resistant to current therapies and can survive when other cancer cells die—making them important treatment targets.
Led by Princess Margaret Cancer Centre Scientist Dr. Steven Chan, the research team conducted a screen of more than 100 drugs known to affect metabolism to find ones that selectively killed leukemic stem cells. Their findings revealed that drugs known as nicotinamide phosphoribosyltransferase (NAMPT) inhibitors were top candidates.
“Unlike normal blood stem cells, leukemic stem cells appear to rely heavily on the NAMPT enzyme to survive. The NAMPT inhibitors that we identified appear to kill leukemic stem cells by disrupting the pathways required for lipid metabolism,” says Dr. Chan.
When the research team treated two laboratory models of acute myeloid leukemia using cells derived from patients with NAMPT inhibitors, leukemia stem cells were much more susceptible to cell death than normal blood stem cells. “This is exciting because our data suggest that NAMPT inhibitors can be used to kill leukemic stem cells without affecting the normal blood system,” says Dr. Chan.
The team focused their experiments on a specific NAMPT inhibitor, known as KPT-9274, which is currently in clinical trials for other types of cancers. In three experimental models of acute myeloid leukemia, treatment with KPT-9274 was effective at killing leukemic stem cells; however, tumour growth in one model remained, suggesting that leukemic stem cells can become resistant to the treatment.
Dr. Chan and his colleagues analyzed the cells that had developed resistance and found that a protein, known as the sterol regulatory-element binding protein (SREBP) became activated when exposed to KPT-9274. Explains first author Amit Subedi, “When we silenced SREBP genes in these cells and treated them with KPT-927, we were able to overcome resistance.”
The team then searched for approved drugs that inhibit SREBP pathways, which led them to the discovery of dipyridamole, a drug used for preventing secondary stroke. The drug combination, when tested in experimental models, killed higher levels of leukemia stem cell than each drug alone and overcame drug resistance.
Comments Dr. Chan, “These results are promising. Future prospective clinical trials are an important next step to validating these findings and building out a more complete picture of the vulnerabilities of acute myeloid leukemia and ways to stamp it out.”
This work was supported by the Acute Leukemia Translational Research Initiative from the Ontario Institute for Cancer Research, the Leukemia Research Foundation, the Canadian Institutes of Health Research and The Princess Margaret Cancer Foundation. J Dick holds a Tier I Canada Research Chair in Stem Cell Biology.
Subedi A, Liu Q, Ayyathan DM, Sharon D, Cathelin S, Hosseini M, Xu C, Voisin V, Bader GD, D’Alessandro A, Lechman ER, Dick JE, Minden MD, Wang JCY, Chan SM. Nicontinamide phosphoribosyltransferase inhibitors selectively induce apoptosis of AML stem cells by disrupting lipid homeostasis. Cell Stem Cell. Epub Ahead of Print

Lead author Dr. Steven Chan, Scientist at Princess Margaret Cancer Centre.




