A study from the Princess Margaret Cancer Centre (PM) has uncovered a surprising way that dying cancer cells weaken the immune system, making cancer therapies less effective. The research team, led by Dr. Tracy McGaha, hopes that this information can be used to help improve the effectiveness of different types of therapies.
Many cancer treatments work by activating the immune system to fight tumours. However, this immune response is not always strong enough to fully kill the cancer or prevent it from recurring. One reason may be that dying cancer cells send signals that suppress the immune system, making treatments less effective.
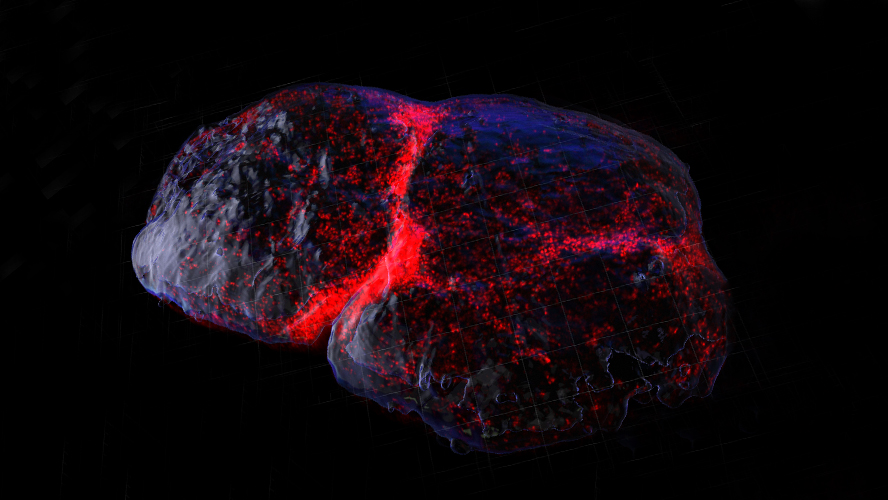
Previous studies found that dying tumour cells can affect tumour-draining lymph nodes (TDLNs)—special lymph nodes where immune responses to cancer usually begin—and weaken the immune system’s ability to fight cancer.
Little is known about the exact mechanisms that take place in TDLNs in response to signals sent by dying tumour cells. To investigate this further, the research team examined what happens in the TDLN following cancer treatments.
The team found that after treatments like chemotherapy or immunotherapy, certain immune cells called macrophages (specifically, medullary sinus macrophages) clean up dead tumour cells and release a protein called IL-33. This protein then drives the body’s resistance to these therapies.
IL-33 activates another group of immune cells called regulatory T cells, which then travel to the tumour and block the immune cells that normally kill cancer. Importantly, the researchers found that blocking or removing IL-33 boosted the immune system’s ability to fight cancer and improved therapeutic responses.
The team then investigated whether IL-33 expression correlates with disease state and outcomes in human cancer. They discovered that higher levels of IL-33 were linked to more severe cancer, and that changes in certain genes related to IL-33 could help predict outcomes in people with melanoma.
These findings open the door to new combination therapies that could enhance the effectiveness of existing cancer treatments by removing this hidden immune roadblock.

(L-R) Dr. Sara Lamorte, first author of the study and Dr. Tracy McGaha, senior author of the study.
Dr. McGaha’s research team also recently reviewed how macrophages behave in tumours and how their roles are linked to their metabolism. This article examines how treatments targeting macrophages might change their activity and metabolism.
The first author of this study is Dr. Sara Lamorte, Scientific Associate at the Princess Margaret Cancer Centre.
The senior author of this study is Dr. Tracy McGaha, Senior Scientist at the Princess Margaret Cancer Centre. Dr. McGaha is a Professor in the Department of Immunology at the University of Toronto.
This work was supported by the National Institutes of Health, Medicine by Design, the Canadian Institutes of Health Research, the Canada Foundation for Innovation, and The Princess Margaret Cancer Foundation.
Drs. Sara Lamorte and Tracy McGaha have filed a provisional patent related to the work reported in the manuscript ‘‘Targeting IL-33 for cancer therapy”.
Lamorte S, Quevedo R, Jin R, Neufeld L, Liu ZQ, Ciudad MT, Lukhele S, Bruce J, Mishra S, Zhang X, Saeed ZK, Berman H, Philpott DJ, Girardin SE, Harding S, Munn DH, Mak TW, Karlsson MCI, Brooks DG, McGaha TL. Lymph node macrophages drive immune tolerance and resistance to cancer therapy by induction of the immune-regulatory cytokine IL-33. Cancer Cell. 2025 Mar 5:S1535-6108(25)00069-8. doi: 10.1016/j.ccell.2025.02.017.




