Home page Description:
Novel method developed at UHN could lead to safer stem cell-derived diabetes treatments.
Posted On: August 25, 2017
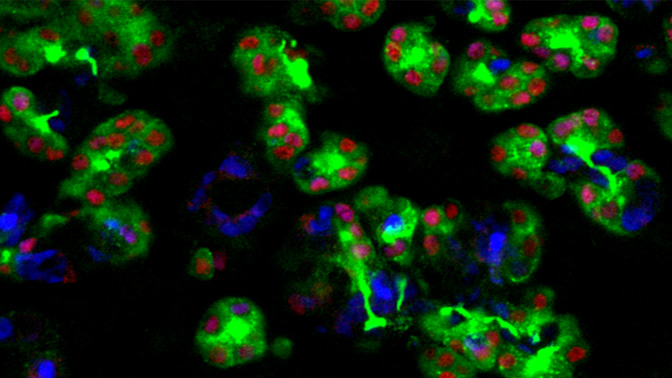
Image Caption:
The insulin-producing beta cells generated in this study (pictured above) may hold the key to future curative therapies for diabetes.
Scientists at TGHRI and the McEwen Centre for Regenerative Medicine have used a novel method to purify cells that develop into insulin-producing cells from human stem cells, paving the way for new therapies and safer transplants in patients with type 1 diabetes.
In work published in Nature Communications today, a team led by Dr. Maria Cristina Nostro, Scientist at TGHRI and the McEwen Centre for Regenerative Medicine Harry Rosen Chair in Diabetes Regenerative Medicine Research, identified a specific marker found on the cell surface of pancreatic progenitor cells, which allowed them to generate pure pancreatic progenitor cells from human pluripotent stem cells and demonstrate how these purified cells could produce beta cells for diabetes treatment.
Pluripotent stem cells have the potential to differentiate into more than 200 different cell types that make up every tissue and organ in the body. They also have the potential to create an endless supply of insulin-producing beta cells, found in the pancreas.
Finding ways to restore destroyed beta cells in the pancreas in patients with type 1 diabetes, or even restore their function in those with type 2 diabetes, is a “holy grail” in diabetes research. Although transplantation of islets from deceased donors has shown that cell replacement therapy—along with immunosuppression—restores beta cell function and decreases the number of insulin injections needed, there are still a number of hurdles.
Widespread use of islet cell transplantation for patients with type 1 diabetes is hampered by the limited supply and quality of donor islets and the effects of immunosuppression medication. The requirement for two to three donors per transplantation and the scarcity of donors has launched a world-wide search for an alternative source of beta cells. Laboratories are in a race to try and find ways to generate large numbers of functioning, insulin-producing beta cells that are safe and pure.
In their quest to purify and generate large quantities of beta cells, the researchers set out to find a highly specific and new marker on the human pancreatic progenitor cell, because generating these specific cells from human stem cells can be challenging and variable. Pancreatic progenitor cells are able to generate insulin-producing beta cells.
Dr. Nostro teamed up with Dr. Thomas Kislinger, a Senior Scientist at PM Cancer Centre and Professor in the Department of Medical Biophysics at the University of Toronto. Together they developed a way to identify markers that would help them distinguish the pancreatic progenitors from cells that lacked the potential to generate beta cells.
“This is of particular importance, as it provides a way to eliminate contaminants,” says Dr. Nostro, who is also an Assistant Professor in the Department of Physiology at the University of Toronto. “The long-term goal is to cure type 1 diabetes with transplants of insulin-producing cells, so it is crucial to have pure cells that we can use for these and other therapies.”
The researchers used a specific antibody-based and magnetic technique to isolate the pancreatic progenitors using their newly identified marker. A specific antibody which binds to the marker on the surface of the pancreatic progenitors was linked to a magnetic bead. A magnet was then used to purify the pancreatic progenitors from other cells.
“Now we have a system that allows us to quantify and control the purity of the cells that will enter clinical trials for the treatment of type 1 diabetes,” says Dr. Nostro.
In Canada, more than 3 million people live with diabetes. It is estimated that this number will grow to 4.2 million by 2020. Diabetes and its complications constitute a serious financial burden for the publicly funded health care system. Direct health care costs due to diabetes and its complications have been estimated at $3 billion for 2015.
Moreover, people with diabetes are more than three times more likely to be hospitalized with cardiovascular disease, 12 times more likely to be hospitalized with end-stage renal disease and more than 20 times more likely to be hospitalized for a non-traumatic lower limb amputation compared to the general population.
For this project, the team collaborated with scientists at Vanderbilt University, Oregon Health and Science University and Sunnybrook Research Institute.
This work was supported by the McEwen Centre for Regenerative Medicine and the Toronto General & Western Hospital Foundation, the Banting and Best Diabetes Centre, the Canadian Institutes of Health Research, the Ontario Ministry of Health and Long-Term Care, the National Institutes of Health, the Juvenile Diabetes Research Foundation (JDRF), the US Department of Veterans Affairs, and the Vanderbilt Diabetes Research and Training Center.
This story originally appeared on www.uhn.ca
TGHRI Scientist Dr. Maria Cristina Nostro gets ready to look at pancreatic progenitor cells that develop into insulin-producing cells from human stem cells.




