Looking at things from a different angle can often lead to new and better solutions. That’s because a fresh perspective can help to inspire creativity, innovative thinking and collaboration.
It’s also why Dr. Cristina Nostro and her team recently embarked on a new collaborative project to solve a particularly difficult research problem: how to reliably isolate a specific pancreatic cell type capable of improving current treatments for type I diabetes.
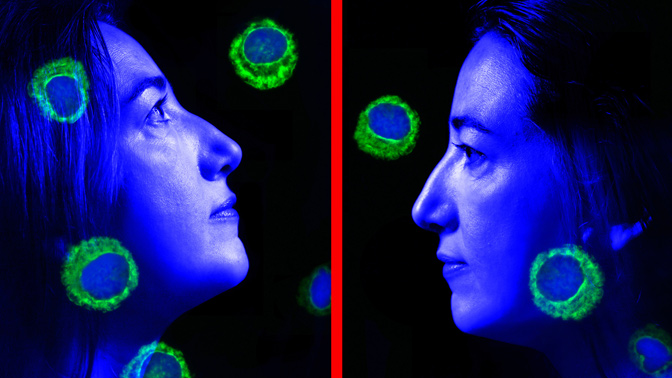
Type I diabetes is a chronic condition in which cells in the pancreas—known as beta cells—are destroyed so little to no insulin is produced. Without insulin, the body is unable to keep blood sugar levels within a healthy range. When blood sugar levels remain consistently high for a prolonged period of time, serious conditions can develop, including heart disease, vision loss, kidney disease and nerve damage.
Transplanting healthy beta cells into the pancreas can restore insulin production and decrease the number of insulin injections needed to maintain normal sugar levels. However, widespread use of this treatment is hampered by a limited supply of donor beta cells for transplantation.
Using stem cells, Dr. Nostro has addressed this issue by developing a reproducible method for generating large numbers of cells that can safely give rise to insulin-producing beta cells. The technique, which mimics what occurs during pancreas development, forces stem cells to mature into daughter stem cells (pancreatic progenitors) that then develop into insulin-producing beta cells.
Unfortunately, the technique also produces progenitors that mature into cells that do not produce insulin. The problem: these contaminating progenitors need to be removed before the therapeutic insulin-producing cells can be safely used in the clinic.
This new approach will help us to develop safer stem cell therapies for diabetes.”
-Dr. Cristina Nostro
Dr. Nostro teamed up with Dr. Thomas Kislinger to explore an entirely new approach to solving this problem. Together they identified specific proteins that are found on the surface of the pancreatic progenitors. They then used one of the proteins—known as Glycoprotein 2—to isolate the pancreatic progenitors and remove the contaminating cells. This allowed them to not only control the number but also the purity of the newly generated insulin-producing cells.
“Our long-term goal is to cure type I diabetes using transplants of insulin-producing cells, so it is crucial to have cells that are safe and pure,” explains Dr. Nostro. “The technique we’ve developed provides a better, more reliable method for generating large quantities of these cells for use in the clinic.”





