By: Joe Walton, ORT Times Writer
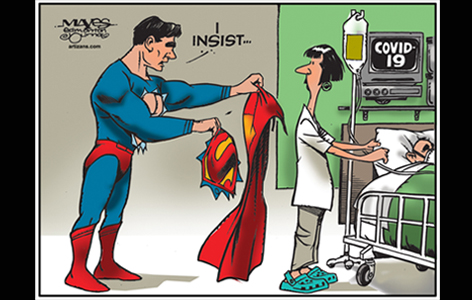
Protecting healthcare workers facing COVID-19 on the frontlines of emergency departments (EDs) and intensive care units (ICUs), is a critical part of our pandemic response.
With looming shortages in personal protective equipment, and a potential vaccine still many months away, UHN researchers are hopeful that hydroxychloroquine, a widely available, ‘World War II era’ malaria drug, might protect at-risk caregivers. Their strategy, vetted in the fight against the human immunodeficiency virus (HIV), is to treat healthy individuals in what is known as pre-exposure prophylaxis, or PrEP.
"If we start to lose too many healthcare workers in the ED and ICU, the system is at risk of collapse…we need to prioritize our approach to the understanding of things that will protect them,” says Dr. Kevin Kain, study co-investigator and infectious disease expert at Toronto General Hospital Research Institute (TGHRI).
Fittingly named the HEalth Care Worker pROphylaxis (HEROs) trial, the study, co-led by Dr. Kain and ED physician Dr. Megan Landes, is one of the first randomized, double-blind, placebo-controlled evaluations of hydroxychloroquine. Canadian pharmaceutical giant, Apotex Inc., has agreed to donate drug for this trial.
The PrEP Strategy
Vaccine protection is our best weapon in the fight against viral pathogens. With it, humanity has eradicated, or nearly eradicated once common and horrible diseases like smallpox and polio. Unfortunately, the global HIV pandemic has taught us that even with decades of research and millions of dollars invested, effective vaccines are never guaranteed.
In 1995, Dr. Che-Chung Tsai at the Regional Primate Research Center in Seattle published one of the first reports demonstrating that a medication, taken either before or just after exposure to HIV could prevent infection from taking hold. Despite this success, another decade of research would be needed to convince regulators that PrEP was a viable strategy for blocking HIV transmission.
The United States Food and Drug Administration (FDA) approved once-daily Truvada, for use in high-risk populations to prevent HIV infection in 2012. Health Canada followed suit in 2016. Today, PrEP is widely available and has been hailed as a “game changer” in battling HIV.
Hydroxychloroquine
Unlike the experimental drugs first tested for HIV prevention, hydroxychloroquine is widely available and has a known safety profile which, Dr. Kain notes, "can greatly accelerate drug development, lowering the cost and rapidly getting it up to scale quickly…But we first need to show it is efficacious." And therein lies the controversy.
Preliminary, lab-based studies suggest some ability for hydroxychloroquine to inhibit the novel coronavirus (SARS-CoV-2). However, clinical evidence is limited and based largely on anecdotal reports. This has not dissuaded some world leaders from advocating widespread use, leading to grave repercussions in supply, resource management and harmful, unnecessary drug side-effects.
The HERO trial, alongside similar international PrEP studies will settle this efficacy debate. Interim results analysis is expected this summer.
Dr. Kain adds, "There are a lot of potentially promising drugs and we need to study them in proper controlled trials to determine if they really work. Right now, we really don't know."




