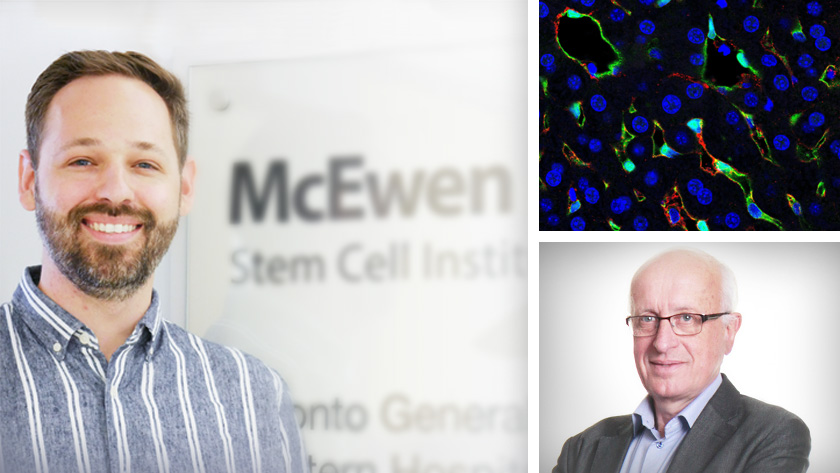
New research from the lab of Dr. Gordon Keller, Senior Scientist and Director of the McEwen Stem Cell Institute, has demonstrated a proof-of-concept cell therapy for hemophilia A in an experimental model.
Hemophilia A is caused by a deficiency in the production of a blood clotting protein known as factor VIII. Individuals with hemophilia A experience internal bleeding, which can cause chronic pain and joint disease. They often require frequent treatment with factor VIII to avoid more serious complications including death.
One of the main sources of factor VIII in the body is a specialized cell type found in the liver known as the liver sinusoidal endothelial cell (LSEC). In this study, Dr. Keller’s team developed a multi-step process to generate LSEC progenitors from a type of stem cell, known as a human pluripotent stem cell, that can develop into any cell in the human body. By manipulating the levels of BMP4 and Activin A—signalling molecules that guide early stages of development—they produced progenitors that were 50 times more efficient at engrafting in the liver than those made with a previously described method.
To test whether the cells could serve as a therapy for hemophilia A, Dr. Keller’s team collaborated with Dr. Antonia Follenzi’s laboratory at the University of Piemonte Orientale in Novara, Italy. Dr. Follenzi’s group has expertise in studying therapeutics for hemophilia A and has access to various experimental models of the disease. For these studies, LSEC progenitors were made in Toronto and then sent to Italy where they were transplanted into experimental models of hemophilia A.
“We wanted to see if these cells could mature into LSECs and make enough factor VIII to improve blood clotting in this experimental model,” says Dr. Blair Gage, post-doctoral fellow in the Keller lab and lead author of the study. “These experiments worked exceptionally well and clearly showed that the human LSECs could engraft in the liver and produce the amount factor VIII required to restore normal blood clotting."
“These findings show that the lab-grown LSECs can function correctly when transplanted into a liver and produce enough factor VIII to make a difference,” says Dr. Gage. “There are remaining hurdles to overcome, such as immune rejection, which is a challenge for many cell therapies. But this study moves us a step closer to developing a cell therapy for people with hemophilia A.”
This work was supported by the University of Toronto’s Medicine by Design Initiative, the Canadian Institutes of Health Research and the UHN Foundation. Dr. Gordon Keller is a Professor of Medical Biophysics at the University of Toronto.
Drs. Gage and Keller have filed a patent related to this work. Dr. Keller is a founding investigator and consultant for BlueRock Therapeutics LP, a consultant for VistaGen Therapeutics and a member of the board of Anagenesis Biotechnologies.
Gage BK, Merlin S, Olgasi C, Follenzi A, Keller GM. Therapeutic correction of hemophilia A by transplantation of hPSC-derived liver sinusoidal endothelial cell progenitors. Cell Rep. 2022 Apr 5. doi: 10.1016/j.celrep.2022.110621.
Adapted from https://mbd.utoronto.ca/news/endothelial-cells-hemophilia-a/
Blood clotting proteins such as factor VIII help to stop bleeding after an injury. Individuals with hemophilia A experience excessive internal bleeding because of deficiencies in factor VIII.

